You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
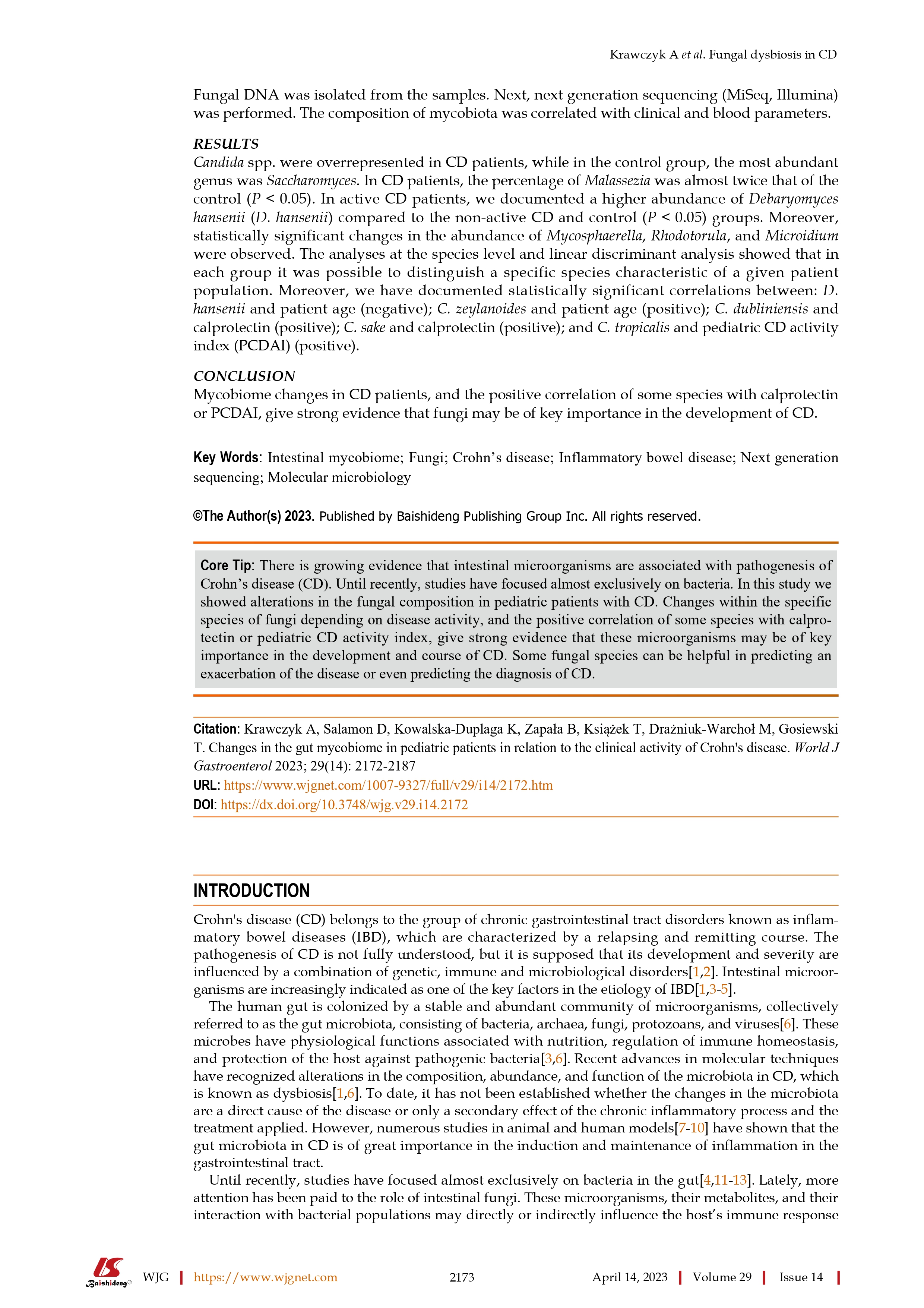
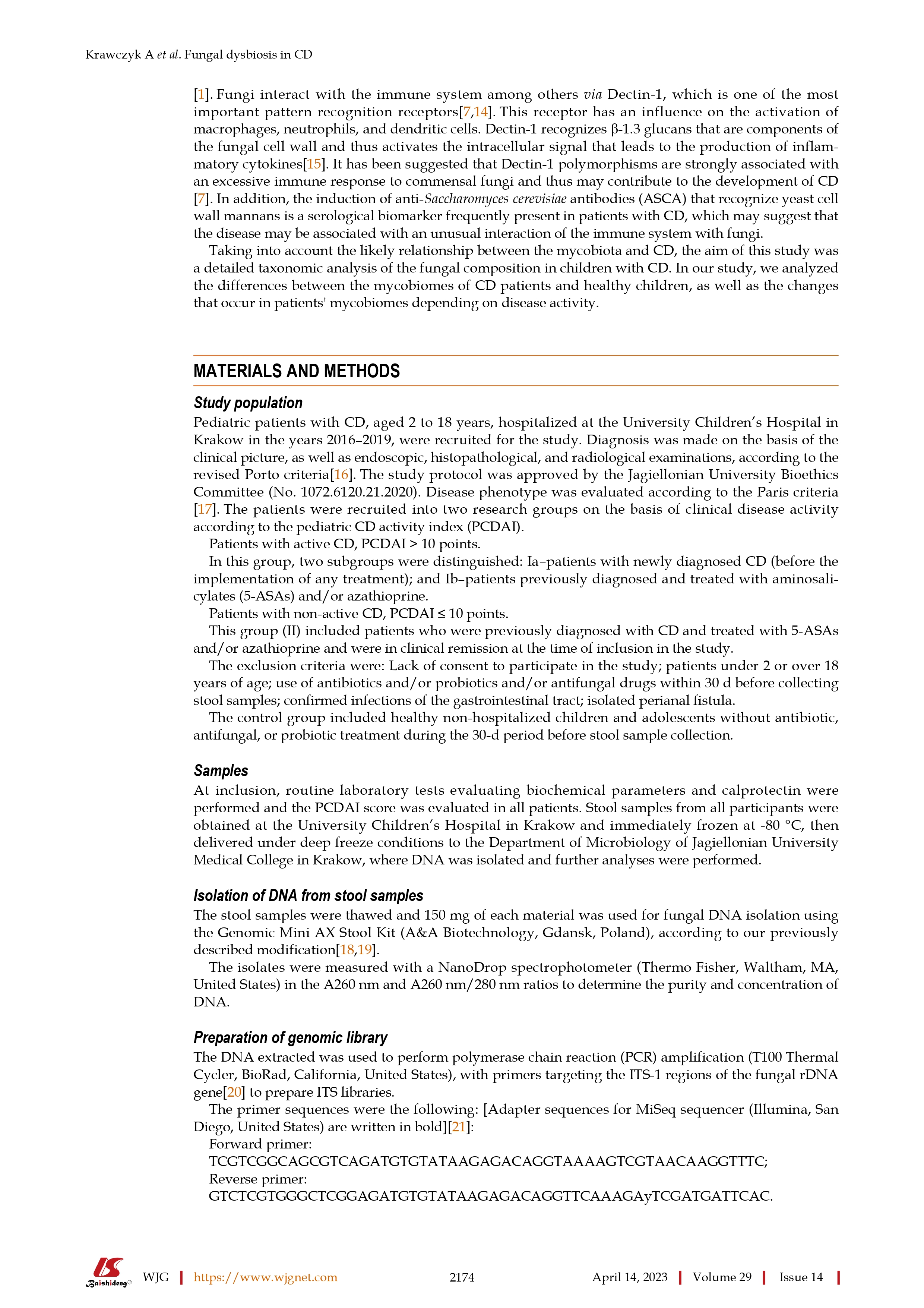
Changes in the gut mycobiome in pediatric patients in relation to the clinical activity of Crohn's disease
- Thread starter kiny
- Start date

Help Support Crohn's Disease Forum:
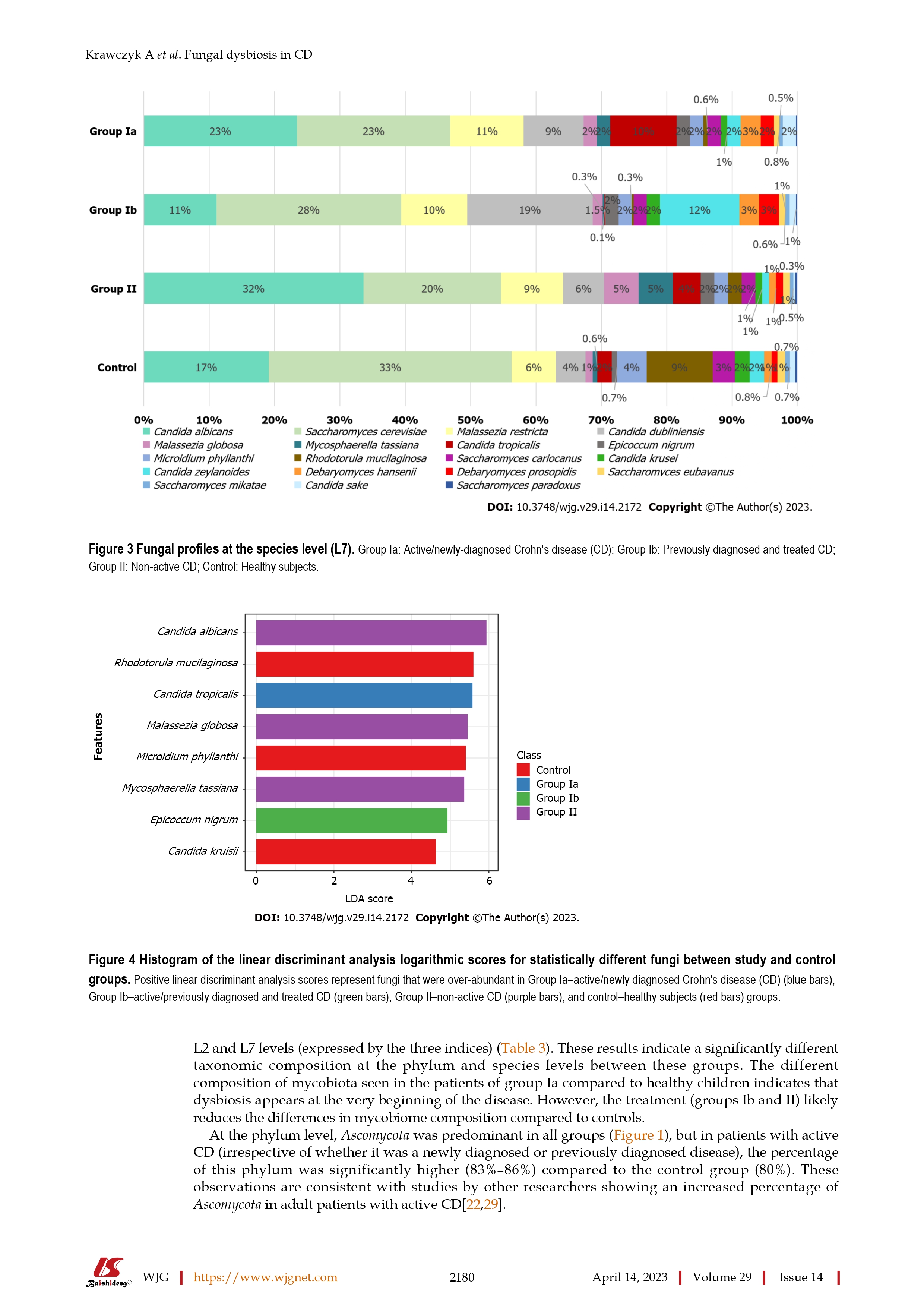
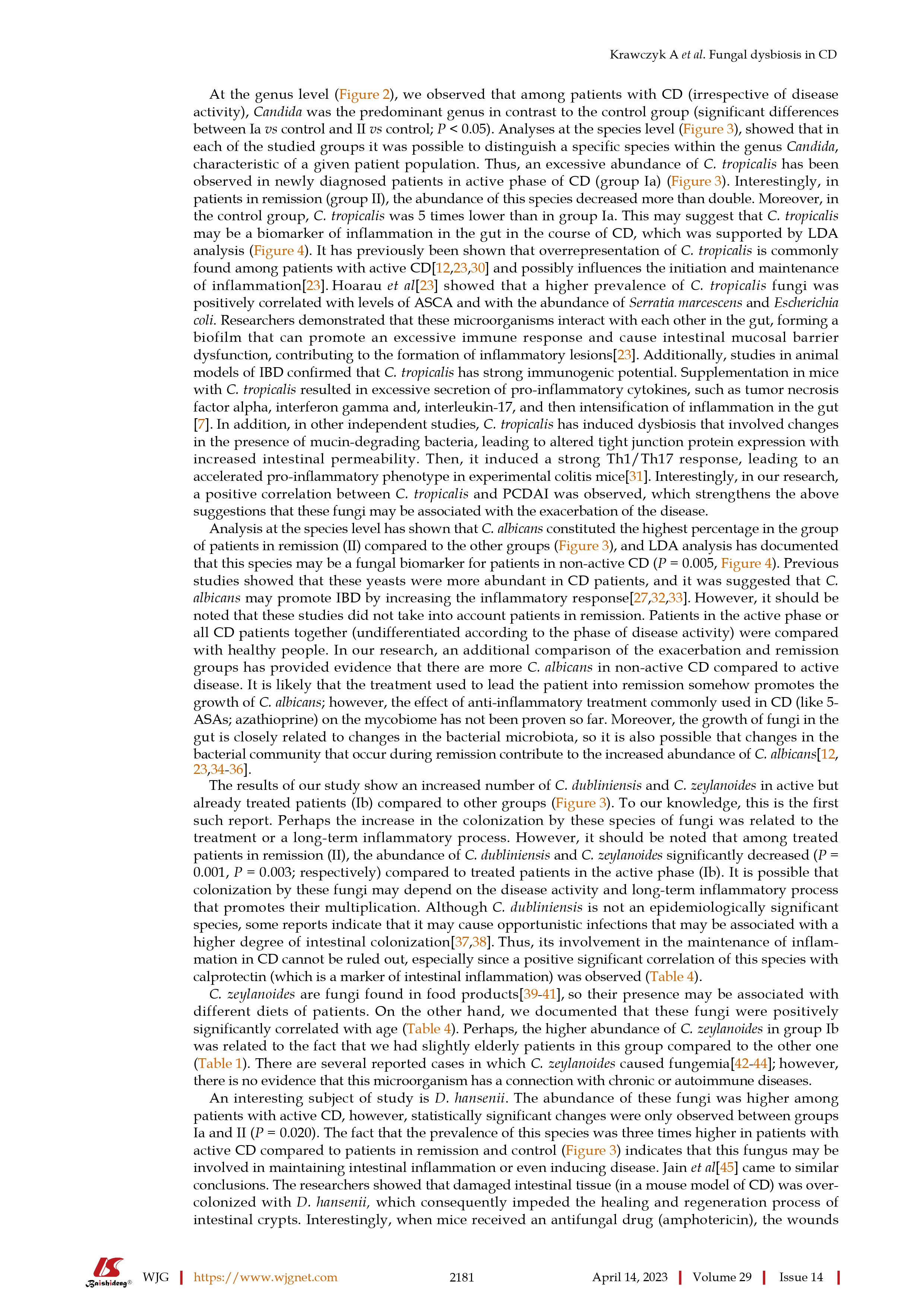
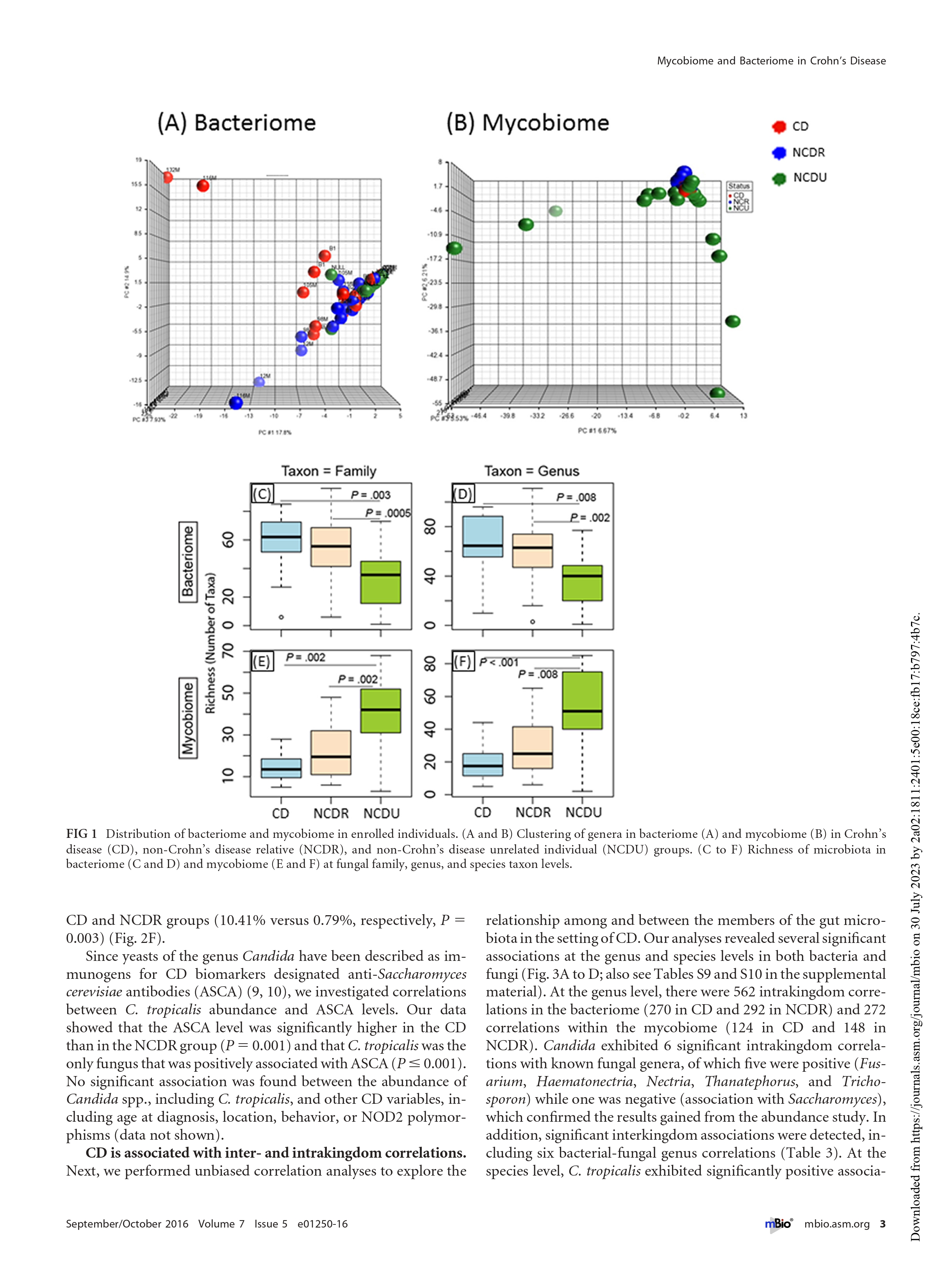
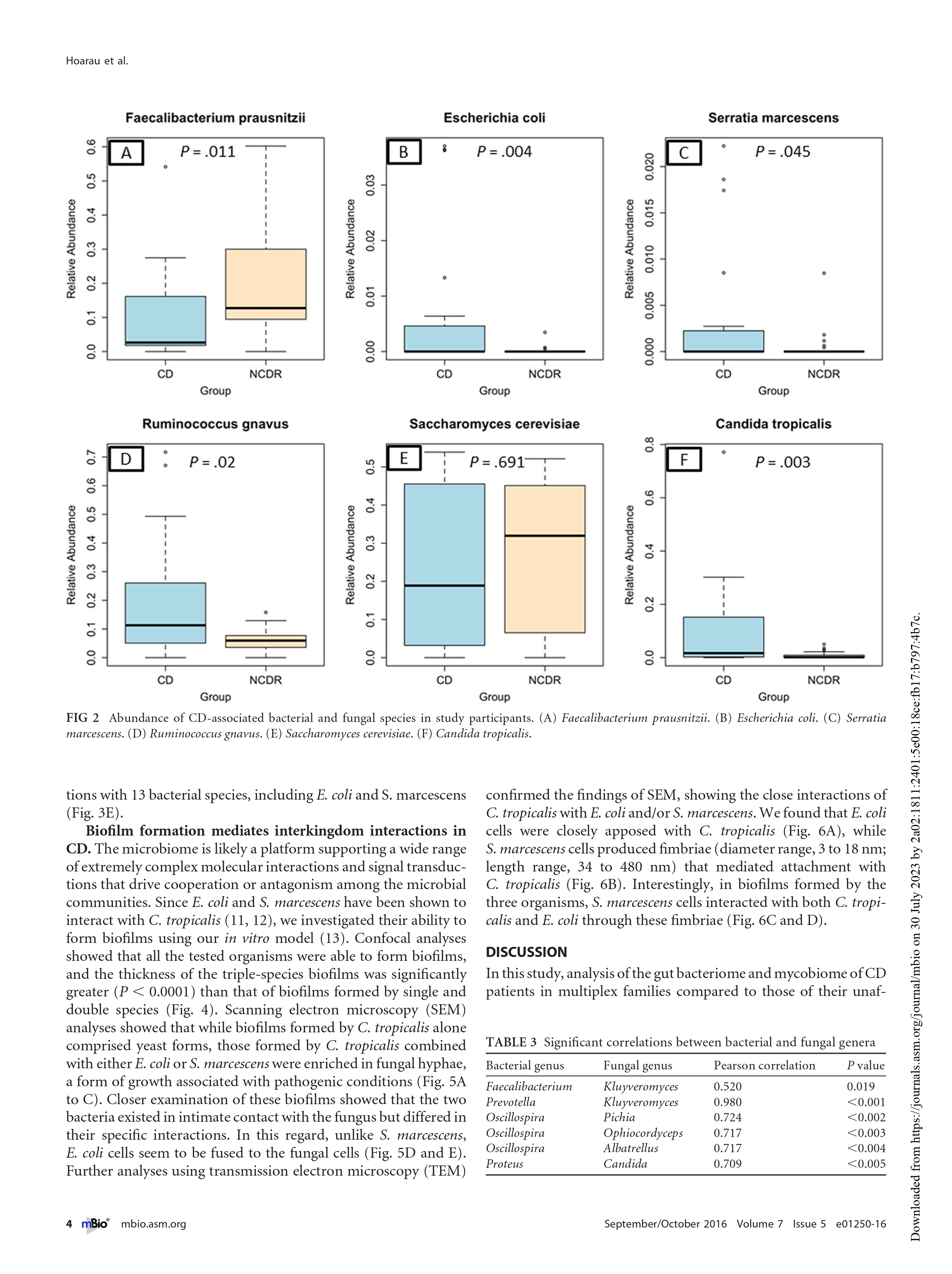
@kiny - Thank you for posting this. This is a long read and perhaps require a few days and I may have to read it multiple times. A quick glance read suggests that candida tropicalis fungus is present in significantly higher quantity in patients with Crohn's than non-Crohn's. Perhaps the unanswered question is if the levels of this fungi are higher because of Crohn's or do the high levels lead to Crohn's. I suppose the next step is to either find a way to normalize the candida tropicalis levels.
@kiny - Perhaps the unanswered question is if the levels of this fungi are higher because of Crohn's or do the high levels lead to Crohn's. I suppose the next step is to either find a way to normalize the candida tropicalis levels.
That's the unanswered question for pretty much every derangement of the of the gut organisms observed in Crohn's: is the derangement a cause of or an effect of the Crohn's?
Hi @Scipio sometimes I think the answer to it may not be so important whether Crohn's is causing the imbalance or imbalance causing Crohn's. If a way is found to fix the gut microbiome imbalances it will be a huge achievement in terms of treatment and help sufferers of Crohn's. Current treatments such as immunosuppressants target to suppress the immune system and these work in some people but not in all and can have potentially serious adverse impacts and even if there are no adverse impacts, after some time maybe few years, the medications stop being effective. There is research happening in delivering probiotics to the gut. Let's hope that the clinical trials happen soon and are safe and effective forms of treatment.
@Scipio actually I found some research https://medicalxpress.com/news/2021-11-scientists-key-trigger-crohn-disease.html
Perhaps there is a cause of Crohn's which causes the gut microbiome imbalance.
Perhaps there is a cause of Crohn's which causes the gut microbiome imbalance.
I would like to use an analogy - diabetes in children vs diabetes in adults. And with Crohn's, no one knows the root cause. It is highly likely that the causes are different. Having said that, the treatments have got lot of commonalities.Why is pediatric Crohn's talked about like its a totally different disease to what adults have? It's strange that they seperate the two conditions so much.
I would like to use an analogy - diabetes in children vs diabetes in adults. And with Crohn's, no one knows the root cause. It is highly likely that the causes are different. Having said that, the treatments have got lot of commonalities.
Is diabetes different in children to adults? Thought it was the same for both.
- Joined
- Apr 15, 2012
- Messages
- 14,848
Type I diabetes (children ) is very different from type II diabetes (adults )
https://my.clevelandclinic.org/health/diseases/7104-diabetes
https://my.clevelandclinic.org/health/diseases/7104-diabetes
kiny
Well-known member
- Joined
- Apr 28, 2011
- Messages
- 3,480
Most people with crohn's disease have pubescent or late pubescent age of onset. Ages 13-20. This is a very homogeneous group of people. The large majority have enteritis. Ileal or ileal-colonic inflammation. It's also the group where you see familial and clustering of cases. This age group is still the dominant group of cases. No one is able to explain why, I think it's because of the bloom in ileal peyer's patch activity during puberty.
But recently, there has been an increasing group of people who fall outside of this traditional age group and are being diagnosed with crohn's disease. But differences in disease features have made me doubt we are still talking about the same disease. People diagnosed when they're 30 or 40, tend to have colonic disease, a much less agresssive disease course, and usually don't have penetrating or stricturing disease. Very young kids below the age of 13 have immunological differences since they have completely underdeveloped peyer's patches. If you put me on the spot, I would say this is not the same disease.
But recently, there has been an increasing group of people who fall outside of this traditional age group and are being diagnosed with crohn's disease. But differences in disease features have made me doubt we are still talking about the same disease. People diagnosed when they're 30 or 40, tend to have colonic disease, a much less agresssive disease course, and usually don't have penetrating or stricturing disease. Very young kids below the age of 13 have immunological differences since they have completely underdeveloped peyer's patches. If you put me on the spot, I would say this is not the same disease.
Last edited:
kiny
Well-known member
- Joined
- Apr 28, 2011
- Messages
- 3,480
Sometimes voices argue that there's many subgroups of crohn's disease, inflammation that can apparently manifest itself everywhere, in different age groups, with wildly different clinical and immunological features. I'm not a big fan of these arguments.
The earliest endoscopic clinical signs of crohn's disease are inflamed lymphoid follicles, peyer's patch activity. When you find inflammation in a different segment of the intestine, lacking peyer's patches, in an age group where peyer's patches are inactive...you can't just say "oh, it's yet another subgroup of crohn's disease". No, it's idiopathic intestinal inflammation at that point, not crohn's disease.
The earliest endoscopic clinical signs of crohn's disease are inflamed lymphoid follicles, peyer's patch activity. When you find inflammation in a different segment of the intestine, lacking peyer's patches, in an age group where peyer's patches are inactive...you can't just say "oh, it's yet another subgroup of crohn's disease". No, it's idiopathic intestinal inflammation at that point, not crohn's disease.
Last edited:
Sometimes voices argue that there's many subgroups of crohn's disease, inflammation that can apparently manifest itself everywhere, in different age groups, with wildly different clinical and immunological features. I'm not a big fan of these arguments.
The earliest endoscopic clinical signs of crohn's disease are inflamed lymphoid follicles, peyer's patch activity. When you find inflammation in a different segment of the intestine, lacking peyer's patches, in an age group where peyer's patches are inactive...you can't just say "oh, it's yet another subgroup of crohn's disease". No, it's idiopathic intestinal inflammation at that point, not crohn's disease.
Kiny, what you are describing is the early onset kids, as young as 3 months old that I've seen. They are given the same Crohn's diagnosis and prescribed the same biologics. I don't know about the VEO population's remission rate on biologics but they are definitely lump with the rest of the Crohn's population.
kiny
Well-known member
- Joined
- Apr 28, 2011
- Messages
- 3,480
Right.
I don't think 3 month olds are developing crohn's disease. BB Crohn, Oppenheimer and Dalziel all had different descriptions for the disease but all of them described regional inflammation in the small intestine with or without colonic involvement, first diagnosed in individuals of pubescent age and young adults. Regional enteritis, terminal ileitis, granulomatous disease of the small bowel.
I don't think 3 month olds are developing crohn's disease. BB Crohn, Oppenheimer and Dalziel all had different descriptions for the disease but all of them described regional inflammation in the small intestine with or without colonic involvement, first diagnosed in individuals of pubescent age and young adults. Regional enteritis, terminal ileitis, granulomatous disease of the small bowel.
- Joined
- Apr 15, 2012
- Messages
- 14,848
The veo centers in the US at least are studying the groups of little kids and documenting everything
Although they use the term “crohns” they know the disease behaves very differently and responds to treatment differently
These centers rely on genetics, immunology , rheumatology and Gi as a group effort .
These studies are still on going with nih to share data among centers so they are getting closer to what it truly is
Although they use the term “crohns” they know the disease behaves very differently and responds to treatment differently
These centers rely on genetics, immunology , rheumatology and Gi as a group effort .
These studies are still on going with nih to share data among centers so they are getting closer to what it truly is
Sometimes voices argue that there's many subgroups of crohn's disease, inflammation that can apparently manifest itself everywhere, in different age groups, with wildly different clinical and immunological features. I'm not a big fan of these arguments.
The earliest endoscopic clinical signs of crohn's disease are inflamed lymphoid follicles, peyer's patch activity. When you find inflammation in a different segment of the intestine, lacking peyer's patches, in an age group where peyer's patches are inactive...you can't just say "oh, it's yet another subgroup of crohn's disease". No, it's idiopathic intestinal inflammation at that point, not crohn's disease.
If you define "Crohn's disease" narrowly enough you can probably make it disappear entirely. All the same same people will still get just as sick. And we will still be treating their illness with the same drugs with which we currently treat Crohn's disease, but we simply will be calling it something other than Crohn's. Which adds up to a semantic exercise in defense of the purity of the term "Crohn's disease."
When someone comes down with an inflammatory bowel disease that looks and acts a lot like Crohn's, it's not helpful to tell them they don't don't really have Crohn's because they are too young, or too old, or their Peyer's patches aren't active enough, etc. Not unless kicking them out of the Crohn's club somehow leads to a different and more effective form of therapy - which, with the possible exception of VEO, it currently does not.
kiny
Well-known member
- Joined
- Apr 28, 2011
- Messages
- 3,480
Which adds up to a semantic exercise in defense of the purity of the term "Crohn's disease."
Tuberculosis is endemic in Latin America, with a high incidence rate. 1.5 million peole die from TB each year. It is a non-stop public health crisis with millions of patients.
When someone develops intestinal inflammation, and both crohn's and intestinal TB are suspected, and you need to evaluate the risk of using immunosuppressants, you better believe that age-of-onset and disease location are not just "an exercise in semantics".
Disease location, and age-of-onset matter. It matters for diagnostic purposes, histology, treatment and evaluating outcomes.
Dalziel realized the patients suspected of having TB had chronic enteritis that was different from TB, because he noticed the age of onset and disease location of patients was similar, and different from TB. "semantics" saved those patients.
Last edited:
kiny
Well-known member
- Joined
- Apr 28, 2011
- Messages
- 3,480
All the same same people will still get just as sick. And we will still be treating their illness with the same drugs
We don't treat everyone with "the same drugs". Disease loaction and age-of-onset are always used in evaluating treatment, because it does lead to more effective therapy.
People with early age-of-onset have a higher chance of a more aggressive ileal disease that is perforating and leads to strictures. For someone who develops colonic disease at a later age, these risks are much lower.
We also know treatments like infliximab are better at treating perforating disease than other treatments.
Age of onset in pubescent patients tends to be familial, there is a higher chance these patients have genetic PRR mutations, which requires more aggressive therapy because these patients have a higher chance of strictures.
Disease location also impacts the use of nutritional therapy. We know EN tends to be more effective in patients with ileitis.
This is not semantics.
Last edited:
kiny
Well-known member
- Joined
- Apr 28, 2011
- Messages
- 3,480
@kinyPerhaps the unanswered question is if the levels of this fungi are higher because of Crohn's or do the high levels lead to Crohn's. I suppose the next step is to either find a way to normalize the candida tropicalis levels.
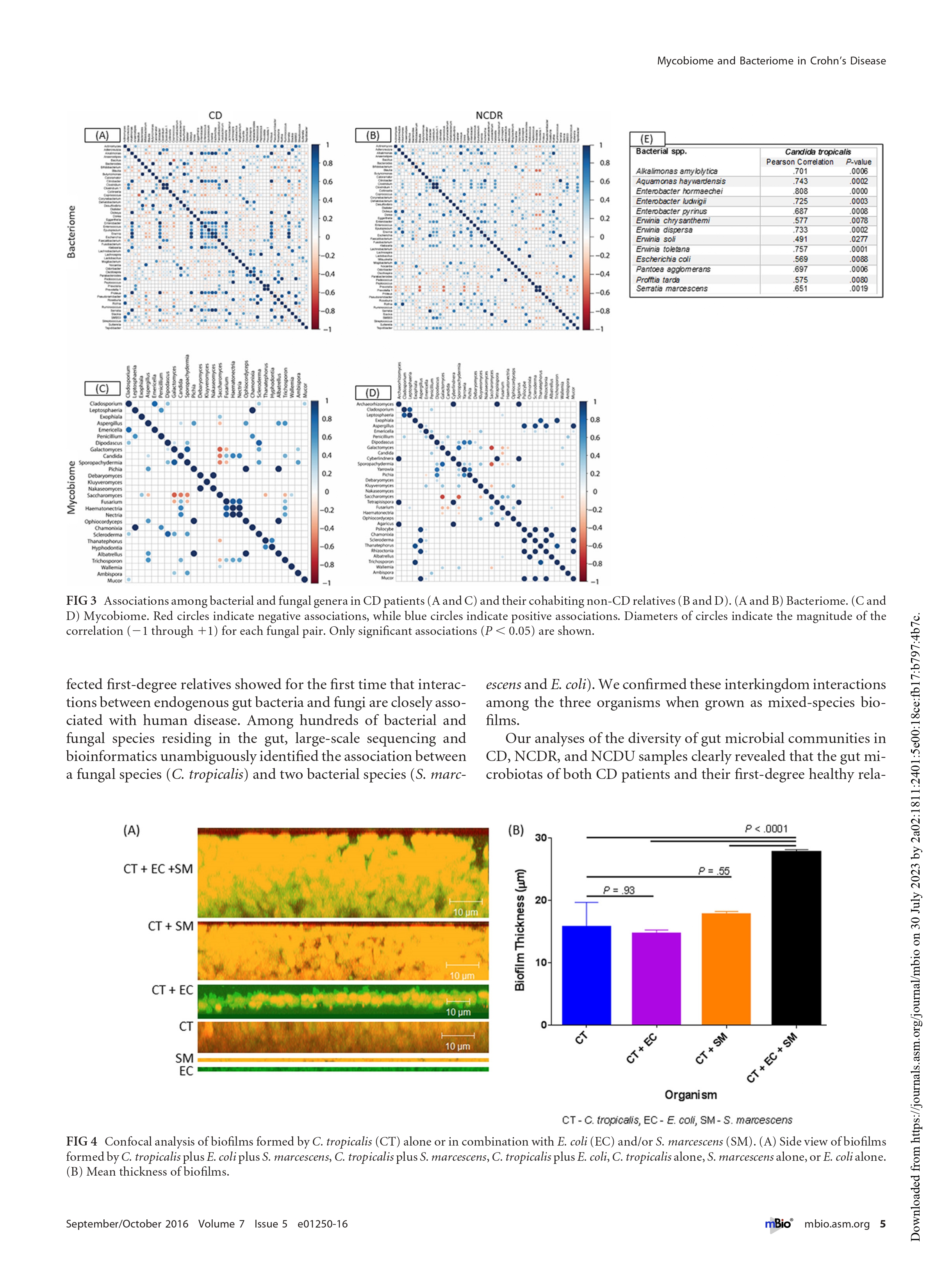
Many of these differences in fungal populations compared to control are independent of inflammation and disease status. But when these populations bloom they could trigger inflammation.
50 percent of caucasians with crohn's disease have at least 1 or more NOD2 mutation. Expressed by macrophages and paneth cells (ileal paneth cells, disease location matters). Bacterial and fungal cell walls activate NOD2. It seems natural that the mycobiome is different in patients with this NOD2 mutation, regardless of disease status.
It's interesting to look at oral fungal populations too, because it's possible these fungal populations are chronically ingested with saliva and end up blooming in the intestine. There's an oral link, people with crohn's disease have abnormally high levels of aphtous ulcers in their mouths.
kiny
Well-known member
- Joined
- Apr 28, 2011
- Messages
- 3,480
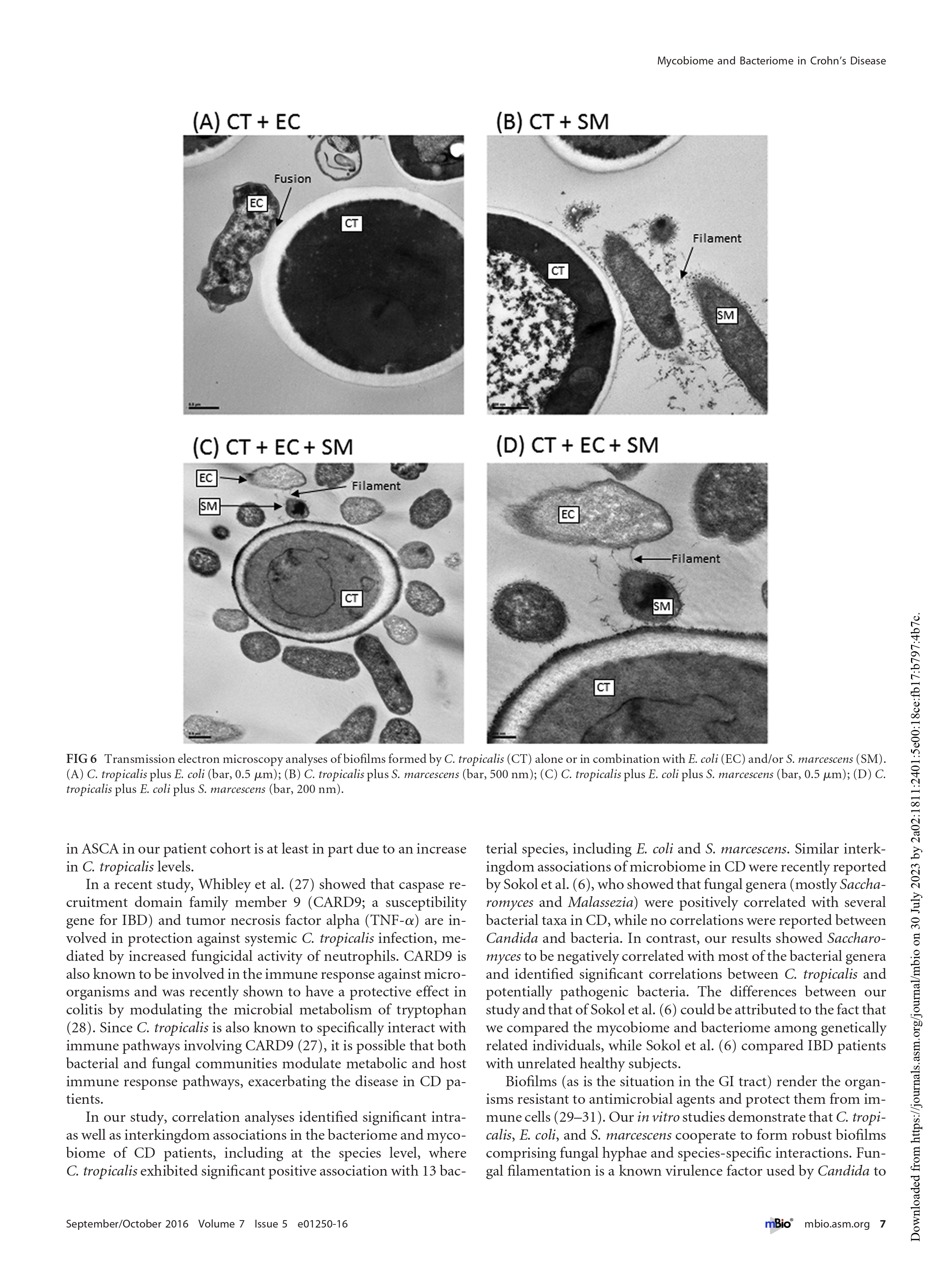
Keep in mind that the microbiota and mycobiome are communicating vessels. Dietary changes, use of antibiotics and immune status all affect both. Colonisation of these communities is self limiting and nutrient dependent. Someone who argues EN works by modulating fungal populations has an argument that is just as valid as someone arguing it modulates Enterobacteriaceae such as species of invasive E coli species or its close relative salmonella.
Rutgeerts showed that "something" larger than 0.22 micron, which is present in the fecal stream, activates lamina propria macrophages and results in inflammation. This could be bacteria, fungi, or large dietary particles.
Fungi, much larger than 0.22 micron, much larger than bacteria, pose a challenge to macrophages once they enter tissue, particularly in patients that would have PRR mutations that would prevent fungal wall recognition, like is the case with NOD2 in crohn's disease patients.
Rutgeerts showed that "something" larger than 0.22 micron, which is present in the fecal stream, activates lamina propria macrophages and results in inflammation. This could be bacteria, fungi, or large dietary particles.
Fungi, much larger than 0.22 micron, much larger than bacteria, pose a challenge to macrophages once they enter tissue, particularly in patients that would have PRR mutations that would prevent fungal wall recognition, like is the case with NOD2 in crohn's disease patients.
Last edited:
Keep in mind that the microbiota and mycobiome are communicating vessels. Dietary changes, use of antibiotics and immune status all affect both. Colonisation of these communities is self limiting and nutrient dependent. Someone who argues EN works by modulating fungal populations has an argument that is just as valid as someone arguing it modulates Enterobacteriaceae such as species of invasive E coli species or its close relative salmonella.
Rutgeerts showed that "something" larger than 0.22 micron, which is present in the fecal stream, activates lamina propria macrophages and results in inflammation. This could be bacteria, fungi, or large dietary particles.
Fungi, much larger than 0.22 micron, much larger than bacteria, pose a challenge to macrophages once they enter tissue, particularly in patients that would have PRR mutations that would prevent fungal wall recognition, like is the case with NOD2 in crohn's disease patients.
When you starve out the fungi, do they actually die or just get weaker like some of the invasive bacteria that we suspect are contributing to the inflammation? I am just wondering what side benefits of EEN are in addition to achieving remission rates on par as steroids?
kiny
Well-known member
- Joined
- Apr 28, 2011
- Messages
- 3,480
When you starve out the fungi, do they actually die or just get weaker like some of the invasive bacteria that we suspect are contributing to the inflammation? I am just wondering what side benefits of EEN are in addition to achieving remission rates on par as steroids?
They should, they're nutrient limited just like bacteria. Fungi absorb what other organisms can't, they can break down cellulose and lignin. That's why trees have barks right, or they would all get eaten by the fungi. EN doesn't have cellulose, fibers, it surely has an impact on fungal populations.
kiny
Well-known member
- Joined
- Apr 28, 2011
- Messages
- 3,480
I would like to know why people with crohn's disease develop aphthous ulcers. They tend to coincide with intestinal inflammation. When you look at these oral lesions, bacterial populations don't seem out of the ordinary. When patients point out the mouth ulcers, the conclusion is usually that it's idiopathic or it's just a manifestation of the disease. That doesn't explain much, mouth ulcers are common in crohn's disease, manifestation in the upper GI tract are otherwise incredibly uncommon in patients. Fungi have been known to cause oral lesions, and are readily isolated from patient saliva.
kiny
Well-known member
- Joined
- Apr 28, 2011
- Messages
- 3,480
Crohn's disease does not exist in a sterile environment. We can't recreate the conditions for inflammation in a sterile environment. Mouse models stop working. Immunological models no longer make sense. There's no babies with crohn's disease and there never will be, their gut is not colonized and sterile, or extremely close to sterile.
Crohn's disease manifests itself in the 3 places in the body that have the highest concentration of bacteria and fungi. Ileum. Colon. Mouth. It's not a coincidence that that's where the majority of our immune cells hang out too. Outside of lymph nodes, nowhere is the concentration of macrophages higher. The body built an express highway for neutrophils to get to the intestine. The immune cells are where the bugs are, that's the intestine. The aphthous ulcers in crohn's disease patients likely hide some clues that could unravel the cause of intestinal inflammation.
Crohn's disease manifests itself in the 3 places in the body that have the highest concentration of bacteria and fungi. Ileum. Colon. Mouth. It's not a coincidence that that's where the majority of our immune cells hang out too. Outside of lymph nodes, nowhere is the concentration of macrophages higher. The body built an express highway for neutrophils to get to the intestine. The immune cells are where the bugs are, that's the intestine. The aphthous ulcers in crohn's disease patients likely hide some clues that could unravel the cause of intestinal inflammation.
Last edited:
kiny
Well-known member
- Joined
- Apr 28, 2011
- Messages
- 3,480
Rutgeerts used 0.22 micrometer to filter the fecal stream, and showed all inflammation subsides and the intestine heals. He could have used 0.45 just as easily which would have also filtered out fungal populations. But the main idea was to filter out the bacterial population which would all be filtered out at 0.22. You use 0.22 to sterilize, not 0.45, the goal in his study was sterilizing. The idea that fungal population could be involved was not that commonly discussed.
If the epithelial barrier is compromised, all sorts of bacteria, fungi and dietary particles would enter tissue and set off an immune response. Any sort of sterilization, from any filter would make inflammation subside. I don't think treatments that lower bacterial load (like EN) only stop initiation of disease activity, they actively lower the impact and severity of a flare, simply by lowering the amount of foreign antigen.
If the epithelial barrier is compromised, all sorts of bacteria, fungi and dietary particles would enter tissue and set off an immune response. Any sort of sterilization, from any filter would make inflammation subside. I don't think treatments that lower bacterial load (like EN) only stop initiation of disease activity, they actively lower the impact and severity of a flare, simply by lowering the amount of foreign antigen.
Last edited:
Can you share which centres are doing research on VEO CROHN'S disease? And any idea by when they will come back with their findings?The veo centers in the US at least are studying the groups of little kids and documenting everything
Although they use the term “crohns” they know the disease behaves very differently and responds to treatment differently
These centers rely on genetics, immunology , rheumatology and Gi as a group effort .
These studies are still on going with nih to share data among centers so they are getting closer to what it truly is
- Joined
- Apr 15, 2012
- Messages
- 14,848
Stanford and children’s hospital of Philadelphia (chop) have veo clinics
Chop at least is part of the nih database in the US
Not sure of other centers
They feed genetics of the kids and parents of veo
Immunology /rheumatology/Gi and genetics all review the kids abd follow them to see if any patterns are there
Not sure when the genetic study will be published with nih
Chop at least is part of the nih database in the US
Not sure of other centers
They feed genetics of the kids and parents of veo
Immunology /rheumatology/Gi and genetics all review the kids abd follow them to see if any patterns are there
Not sure when the genetic study will be published with nih
I agree. If the epithelial integrity is breached, it will allow all sorts of bacteria, fungi to get into the gut. However, if there is a way to restore the balance during that time, it will be extremely useful because diets such as EEN, CDED are trying to do just that. So far the researchers haven't found a way to restore the balance via medication or oral ingestion of good gut bacteria. There was some research done by Washington State university but no update since then on human trials.Rutgeerts used 0.22 micrometer to filter the fecal stream, and showed all inflammation subsides and the intestine heals. He could have used 0.45 just as easily which would have also filtered out fungal populations. But the main idea was to filter out the bacterial population which would all be filtered out at 0.22. You use 0.22 to sterilize, not 0.45, the goal in his study was sterilizing. The idea that fungal population could be involved was not that commonly discussed.
If the epithelial barrier is compromised, all sorts of bacteria, fungi and dietary particles would enter tissue and set off an immune response. Any sort of sterilization, from any filter would make inflammation subside. I don't think treatments that lower bacterial load (like EN) only stop initiation of disease activity, they actively lower the impact and severity of a flare, simply by lowering the amount of foreign antigen.
kiny
Well-known member
- Joined
- Apr 28, 2011
- Messages
- 3,480
EN use results in decreased diversity, increased dysbiosis . Most gut bacteria can't be cultured, biopsies and stool samples produce drastically different results when trying to map out a microbiome. Trying to figure out which bacterial populations are affected is a pointless endeavour, most studies contradict each other completely. It's not an exact science.
I don't think any of this matters, even if you knew how EN shapes the microbiome, what are you going to do with this info? Give people probiotics? No, because it doesn't work. Whatever dysbiosis happens during EN treatment is simply a response to a drastic dietary change.
What matters is how EN is able to bring down inflammation within days. Perpetual inflammation in crohn's disease is the result of intestinal bacteria that cross the mucus barrier into tissue. EN is a number's game, it limits the amount of nutrients available to these bacteria, drastically brings down bacterial load (EN is highly effective in treating SIBO) and limits the number of lamina propria immune cells that will be involved in the immune response.
I don't think any of this matters, even if you knew how EN shapes the microbiome, what are you going to do with this info? Give people probiotics? No, because it doesn't work. Whatever dysbiosis happens during EN treatment is simply a response to a drastic dietary change.
What matters is how EN is able to bring down inflammation within days. Perpetual inflammation in crohn's disease is the result of intestinal bacteria that cross the mucus barrier into tissue. EN is a number's game, it limits the amount of nutrients available to these bacteria, drastically brings down bacterial load (EN is highly effective in treating SIBO) and limits the number of lamina propria immune cells that will be involved in the immune response.
Last edited:
kiny
Well-known member
- Joined
- Apr 28, 2011
- Messages
- 3,480
I like to push back a bit against the recent trend where each study about the gut microbiome is heralded as some kind of breakthrough that will drastically change the outlook on a host of diseases.
There's a handful of invasive bacteria and fungi we know very well that are particularly good at invading peyer's patches and intestinal cells. E coli (aiec), salmonella, campylobacter, yersinia, malassezia and a few others. When millions of people come down with crohn's disease, it is unlikely that the culprit is going to be an exotic tropical bacteria no one has ever heard of. The worst offenders are well known, they're invasive pathogens and pathobionts and can't be considered as part of the normal microbiome.
It took a century to culture the bacteria behind syphilis. It could take several centuries to map out the gut microbiome. Mapping out the microbiome has cost billions of $, and so far has helped no one. It did help to sell probiotics, which are not useful to treat crohn's disease, or frankly any disease I am aware of.
There's a handful of invasive bacteria and fungi we know very well that are particularly good at invading peyer's patches and intestinal cells. E coli (aiec), salmonella, campylobacter, yersinia, malassezia and a few others. When millions of people come down with crohn's disease, it is unlikely that the culprit is going to be an exotic tropical bacteria no one has ever heard of. The worst offenders are well known, they're invasive pathogens and pathobionts and can't be considered as part of the normal microbiome.
It took a century to culture the bacteria behind syphilis. It could take several centuries to map out the gut microbiome. Mapping out the microbiome has cost billions of $, and so far has helped no one. It did help to sell probiotics, which are not useful to treat crohn's disease, or frankly any disease I am aware of.
I like to push back a bit against the recent trend where each study about the gut microbiome is heralded as some kind of breakthrough that will drastically change the outlook on a host of diseases.
There's a handful of invasive bacteria and fungi we know very well that are particularly good at invading peyer's patches and intestinal cells. E coli (aiec), salmonella, campylobacter, yersinia, malassezia and a few others. When millions of people come down with crohn's disease, it is unlikely that the culprit is going to be an exotic tropical bacteria no one has ever heard of. The worst offenders are well known, they're invasive pathogens and pathobionts and can't be considered as part of the normal microbiome.
It took a century to culture the bacteria behind syphilis. It could take several centuries to map out the gut microbiome. Mapping out the microbiome has cost billions of $, and so far has helped no one. It did help to sell probiotics, which are not useful to treat crohn's disease, or frankly any disease I am aware of.
Why is it difficult to culture these bacteria?
kiny
Well-known member
- Joined
- Apr 28, 2011
- Messages
- 3,480
Because you pull them from their natural environment they need to grow when you isolate them in a petri dish. They might require living in symbiosis with other bacteria to grow, they require the presence of biofilm of other bacteria to grow, they might need signaling from other bacteria, they need specific nutrients, etc. You can only culture a small fraction of bacteria, most can not be cultured.
kiny
Well-known member
- Joined
- Apr 28, 2011
- Messages
- 3,480
Someone would likely argue that you can use molecular techniques to identify some of these bacteria.
But that's not very useful unless you already studied the bacteria through culture. To know what type of bacteria you are dealing with, to know how this bacteria interacts with the intestine, to understand under what conditions it survives, you need to culture them.
"we used a high throughput detection method to determine people with crohn's disease have bacteria that have a genetic signature that belongs to group x,y,z" is not very useful if you have no idea how this bacteria interacts with the host.
We have all this molecular data that isn't useful and doesn't lead to better treatments, because no one has any idea what to do with that data. A bacteria is of interest when you start to define how it interacts with the host, this happened with AIEC for example, reference strain LF82 is well studied.
But that's not very useful unless you already studied the bacteria through culture. To know what type of bacteria you are dealing with, to know how this bacteria interacts with the intestine, to understand under what conditions it survives, you need to culture them.
"we used a high throughput detection method to determine people with crohn's disease have bacteria that have a genetic signature that belongs to group x,y,z" is not very useful if you have no idea how this bacteria interacts with the host.
We have all this molecular data that isn't useful and doesn't lead to better treatments, because no one has any idea what to do with that data. A bacteria is of interest when you start to define how it interacts with the host, this happened with AIEC for example, reference strain LF82 is well studied.
Someone would likely argue that you can use molecular techniques to identify some of these bacteria.
But that's not very useful unless you already studied the bacteria through culture. To know what type of bacteria you are dealing with, to know how this bacteria interacts with the intestine, to understand under what conditions it survives, you need to culture them.
"we used a high throughput detection method to determine people with crohn's disease have bacteria that have a genetic signature that belongs to group x,y,z" is not very useful if you have no idea how this bacteria interacts with the host.
No wonder Crohn's is nearly Impossible to root cause. :/
kiny
Well-known member
- Joined
- Apr 28, 2011
- Messages
- 3,480
The type of bacteria that cause gastroenteritis are mostly foodborne or mycobacteria. By definition, it means they are easy to culture.
E Coli (AIEC), Salmonella, Listeria, Campylobacter, Yersinia. You can all easily culture them or detect them with PCR if you're pressed for time. TB should have been ruled out and is uncommon in the west.
The microbiome and fecal matter is involved in the inflammatory cascade in crohn's disease because these bacteria and undigested particles cross the epithelial barrier into tissue during inflammation. They might not initiate the disease state, but they certainly exacerbate it. This is clear from these fecal transplant studies that can exacerbate inflammation in crohn's disease patients. EN doesn't cure crohn's disease, it just makes the inflammation subside.
Does it help mapping out all these thousands of different commensal bacteria, I don't think it does.
Do all these studies trying to "restore" the microbiome in crohn's disease patients help? No, no one agrees on what a "healthy" microbiome looks like and the treatments to modify the microbiome have been a waste of time or actually hurt patients. Probiotics don't help and fecal transplants just make people way more sick.
E Coli (AIEC), Salmonella, Listeria, Campylobacter, Yersinia. You can all easily culture them or detect them with PCR if you're pressed for time. TB should have been ruled out and is uncommon in the west.
The microbiome and fecal matter is involved in the inflammatory cascade in crohn's disease because these bacteria and undigested particles cross the epithelial barrier into tissue during inflammation. They might not initiate the disease state, but they certainly exacerbate it. This is clear from these fecal transplant studies that can exacerbate inflammation in crohn's disease patients. EN doesn't cure crohn's disease, it just makes the inflammation subside.
Does it help mapping out all these thousands of different commensal bacteria, I don't think it does.
Do all these studies trying to "restore" the microbiome in crohn's disease patients help? No, no one agrees on what a "healthy" microbiome looks like and the treatments to modify the microbiome have been a waste of time or actually hurt patients. Probiotics don't help and fecal transplants just make people way more sick.
- Joined
- Mar 22, 2023
- Messages
- 116
What I am struggling to understand is, does fasting help patients the same degree as EEN in the short term? I have only seen lousy nonsensical studies on this matter. That would at least give us the info if there is something in EEN, or rather, something that isn’t in it, that helps so many people. I am especially interested in this given my intolerance (physical one.. I am one of those weird ones who love their taste) for the tried commercial EEN formulas, to make homemade one, or give other type of liquid diets a try.
- Joined
- Mar 22, 2023
- Messages
- 116
In my personal experience going 2 days on broth liquid does seem to help a lot. But I cannot stop eating longer than that, because I need to be productive on an everyday basis. And every failed experiment with this joke of a disease takes many days to recover from, so I dont really dare to try single ingredients mixed with the liquid.
- Joined
- Apr 24, 2021
- Messages
- 216
I remember the first time I took Enn knocked my crohns into space felt amazing, had over ten years on partial enn living life great, but then it stopped working, crohns is a progressive disease, I'm sure there are studies on enn that has stopped working, maybe is its the damage got a bit worse by a small percentage each year until the enn could no longer control it in my ileum.
In my case it works its highly effective, but the crohns does find a way around it.
You also feel like your getting and absorbing much more nutrition, this in itself helps hugely.
But why enn worked for so long and crohns finds a way around it and stopped working on me, that is puzzling, and a shame as being immune supressd is a different ball game to taking some drinks each day.
100% I can say the enn hit my crohns like a hammer with a nail, controlled it with superior power, then stopped.
Despite 3 months of full enn at around year ten when the effects wore off it never has that same power again as ten years ago.
In my case it works its highly effective, but the crohns does find a way around it.
You also feel like your getting and absorbing much more nutrition, this in itself helps hugely.
But why enn worked for so long and crohns finds a way around it and stopped working on me, that is puzzling, and a shame as being immune supressd is a different ball game to taking some drinks each day.
100% I can say the enn hit my crohns like a hammer with a nail, controlled it with superior power, then stopped.
Despite 3 months of full enn at around year ten when the effects wore off it never has that same power again as ten years ago.
I remember the first time I took Enn knocked my crohns into space felt amazing, had over ten years on partial enn living life great, but then it stopped working, crohns is a progressive disease, I'm sure there are studies on enn that has stopped working, maybe is its the damage got a bit worse by a small percentage each year until the enn could no longer control it in my ileum.
In my case it works its highly effective, but the crohns does find a way around it.
You also feel like your getting and absorbing much more nutrition, this in itself helps hugely.
But why enn worked for so long and crohns finds a way around it and stopped working on me, that is puzzling, and a shame as being immune supressd is a different ball game to taking some drinks each day.
100% I can say the enn hit my crohns like a hammer with a nail, controlled it with superior power, then stopped.
Despite 3 months of full enn at around year ten when the effects wore off it never has that same power again as ten years ago.
10 years is super amazing though.
I agree that Crohn's disease people will have all sorts of bugs because of the fact epithelial barrier is breached. The other problem is that when the intestines are suffering from inflammation, it is not possible for probiotics to reach the intestines. And it is also possible that even if a way is found to administer probiotics where it can reach the gut , it may not work. But what if it works. Even if the probability is low, we should not lose hope.I like to push back a bit against the recent trend where each study about the gut microbiome is heralded as some kind of breakthrough that will drastically change the outlook on a host of diseases.
There's a handful of invasive bacteria and fungi we know very well that are particularly good at invading peyer's patches and intestinal cells. E coli (aiec), salmonella, campylobacter, yersinia, malassezia and a few others. When millions of people come down with crohn's disease, it is unlikely that the culprit is going to be an exotic tropical bacteria no one has ever heard of. The worst offenders are well known, they're invasive pathogens and pathobionts and can't be considered as part of the normal microbiome.
It took a century to culture the bacteria behind syphilis. It could take several centuries to map out the gut microbiome. Mapping out the microbiome has cost billions of $, and so far has helped no one. It did help to sell probiotics, which are not useful to treat crohn's disease, or frankly any disease I am aware of.
It is perhaps one of the biggest challenges of Crohn's disease. How and why does the body find a way around a treatment which has worked in the past?I remember the first time I took Enn knocked my crohns into space felt amazing, had over ten years on partial enn living life great, but then it stopped working, crohns is a progressive disease, I'm sure there are studies on enn that has stopped working, maybe is its the damage got a bit worse by a small percentage each year until the enn could no longer control it in my ileum.
In my case it works its highly effective, but the crohns does find a way around it.
You also feel like your getting and absorbing much more nutrition, this in itself helps hugely.
But why enn worked for so long and crohns finds a way around it and stopped working on me, that is puzzling, and a shame as being immune supressd is a different ball game to taking some drinks each day.
100% I can say the enn hit my crohns like a hammer with a nail, controlled it with superior power, then stopped.
Despite 3 months of full enn at around year ten when the effects wore off it never has that same power again as ten years ago.
kiny
Well-known member
- Joined
- Apr 28, 2011
- Messages
- 3,480
What I am struggling to understand is, does fasting help patients the same degree as EEN in the short term? I have only seen lousy nonsensical studies on this matter. That would at least give us the info if there is something in EEN, or rather, something that isn’t in it, that helps so many people.
If there was something in EN actively suppressing intestinal inflammation, why does EN delivered through intravenous means, bypassing the intestine, work jut as well.
Intravenous feeding for crohn's disease to treat inflammation is rare due to the high risk of infections. If it is used, it is usually to help people with crohn's disease who are severely malnourished, but it is also very effective in lowering inflammation. But what it does show is that it is unlikely that EN's method of action is through changes in the microbiome, or because of the presence of any particular nutrient in EN. There's nothing peculiar about EN outside of its very rapid proximal absorption. The presence of MCT or TGF don't seem to be necessary for EN to be effective, EN solution have been effective for decades to treat crohn's disease. You can read the EN studies from the 80s and the composition of EN, they're very simple high absorption solutions.
When studies compare the effectiveness of EN, they all seem very effective and any differences in effectiveness between brands are incredibly small. EN (028, Modulen, and peptamen) all work. Elemental 028 seems to be a tiny bit more effective than its competitors in some studies, but the difference is incredibly small, all EN are all incredibly effective in lowering inflammation.
EN causes a rapid decrease in bacterial load and the absence of antigenic stimuli and dietary triggers in EN cause inflammation to subside. That's all due to its rapid proximal absorption, not because there is a peculiar ingredient in EN, the ingredient list of EN solution is very boring. EN all consist of a high dextrose equivalent substance, marked as glucose/glucose syrup/high DE maltodextrin, easy to absort fats (high MCT) and protein in the form of casein or whey that are naturally lactose free. That all these nutrients have in common is that they are easily and proximally absorbed, that's what EN was designed to do right, a high absorption solution, it wasn't designed to treat crohn's disease, it's just incredibly effective at it.
What I am struggling to understand is, does fasting help patients the same degree as EEN in the short term?
Crohn's disease often first presents itself as anorexia. The fecal stream is involved in inflammation in crohn's disease, people stop eating because it diminishes the pain they experience. But malnutrition will lead to deficiencies in certain proteins like glutamine that the small intestine desperately needs to maintain epithelial barrier function, these cells are constantly being renewed every few days. There's no reason to try fasting and risk malnutrition, when there's dietary solutions that result in proximal absorption of nutrients, like EN.
Last edited:
- Joined
- Mar 22, 2023
- Messages
- 116
There's no reason to try fasting and risk malnutrition, when there's dietary solutions that result in proximal absorption of nutrients, like EN.
I truly wish that were the case. Last week I have tried the 4th EEN formula that made things significantly worse. And recently I have been doing pre and after calprotectin measurements, so its not just the symptoms. I had to do broth fasting 3 days to get back in ok-ish shape. But, like you say, fasting sucks and it's risky. I wish I knew what particular ingredient is causing me to have this kind of bad reaction, coz my proximal intestine is healthy-ish, and otherwise my Crohn's is considered relatively mild (its in TI). Now I am just desperately experimenting: try an EEN with milk proteins without maltodextrin, without pea proteins and fibers.. try one with maltodextrin, without the other 3... etc. No IgE allergies or anything like that.
but man is it exhausting.. the only thing that seems to work for me for maintenance is SCD without fruits without milk, without too much of anything at once. I had a wonderful 4 months on that before I broke it with alcohol and fruit juices on my wedding. And this time it does not seem to be enough to get me back in full remission. We are even taking a honeymoon to the US in large part to try Kate Farms
I knew there were studies trying to replicate EEN from whole foods. I have a blender and everything at home, so when all commercial formulas have been exhausted I guess I will start to experiment with something of my own. But I wish there were more studies pointing me somewhere, it feels like being the dark.
kiny
Well-known member
- Joined
- Apr 28, 2011
- Messages
- 3,480
SCD tries to mimick EN really. The diet doesn't allow carbohydrates that require enzymes to cleave the double sugar chains, nor does it allow starch. The diet only allows single molecule sugars that readily get absorbed as blood glucose. As the SCD argument goes, a normal diet leads to indigestion and bacterial overgrowth. The recent data suggesting many people with CD have some form of SIBO does lend some credence to this theory. The fact EN is very effective at treating SIBO is also interesting, EN leads to a dramatic reduction in bacterial load, especially in the small intestine.
But SCD studies are mixed, some show improvements, but several do not. While studies on EN consistently show improvement. It's hard to say what someone on SCD actually eats in practice, fructose are also allowed on SCD, while EN are all glucose syrup/maltodextrin based.
But SCD studies are mixed, some show improvements, but several do not. While studies on EN consistently show improvement. It's hard to say what someone on SCD actually eats in practice, fructose are also allowed on SCD, while EN are all glucose syrup/maltodextrin based.
Last edited:
kiny
Well-known member
- Joined
- Apr 28, 2011
- Messages
- 3,480
coz my proximal intestine is healthy-ish, and otherwise my Crohn's is considered relatively mild (its in TI).
It's the case for everyone right. The disease presents itself where the bacteria reside, patchy ileal and colonic manifestation of inflammation.
"the disease can affect any part of the digestive tract" is simply not the case. So called "gastroduodenal crohn's disease" is incredibly rare, often transient, lack granuloma, and doesn't look like crohn's disease at all. Crohn's disease manifests itself in the ileum, colon and mouth as aphthous ulcers, that's where all the bugs are. The presence of bacteria is conditional to properly mimick this disease in rodents, crohn's disease does not exist in sterile environments. Compared to the ileum, the duodenum and stomach is a very sterile and acidic environment, there's no microbiota to speak of in those parts of the GI tract.
Last edited:
If EN is so effective why are adults given prednisone? And if its due to tolerating, why don't they develop better tasting varieties. Seems like a no brainer but instead everyone is given prednisone risking more side effects and further problems.
Feels a bit lazy to go immediately for prednisone.
Feels a bit lazy to go immediately for prednisone.
- Joined
- Apr 15, 2012
- Messages
- 14,848
Adults have issues with not eating solid foods period
Most refuse
It’s not about taste
Een can be done with polymeric formula (boost , ensure etc…)
Typically Gi will call it a success if an adult is willing to go two weeks without solid food
kids are under the guidance of their parents who set the rules which is why een is used more in little kids
Teens are tougher
Most refuse
It’s not about taste
Een can be done with polymeric formula (boost , ensure etc…)
Typically Gi will call it a success if an adult is willing to go two weeks without solid food
kids are under the guidance of their parents who set the rules which is why een is used more in little kids
Teens are tougher
Adults have issues with not eating solid foods period
Most refuse
It’s not about taste
Een can be done with polymeric formula (boost , ensure etc…)
Typically Gi will call it a success if an adult is willing to go two weeks without solid food
kids are under the guidance of their parents who set the rules which is why een is used more in little kids
Teens are tougher
Not willing because old habits die hard or what? I did it before when i had food poisoning, when your unwell enough 2 weeks is nothing lol
It's the case for everyone right. The disease presents itself where the bacteria reside, patchy ileal and colonic manifestation of inflammation.
"the disease can affect any part of the digestive tract" is simply not the case. So called "gastroduodenal crohn's disease" is incredibly rare, often transient, lack granuloma, and doesn't look like crohn's disease at all. Crohn's disease manifests itself in the ileum, colon and mouth as aphthous ulcers, that's where all the bugs are. The presence of bacteria is conditional to properly mimick this disease in rodents, crohn's disease does not exist in sterile environments. Compared to the ileum, the duodenum and stomach is a very sterile and acidic environment, there's no microbiota to speak of in those parts of the GI tract.
By the way what's your view on the MAP bacteria ? You mention its hard to identify which bacteria could be the problem in the gut biome due to how complex it all is, but MAP does cause Johne's disease in cows which has similarities to IBD. Additionally as India and other Asian nations started introducing more dairy into their diet like the west has their rates of IBD are increasing inline with the west... there has always been an understanding that as nations become more developed IBD became more common which often was believed to be due to over sterilising our kitchens etc. Dairy is a major source of MAP - though have read it is also prevalent in the water table in most nations that have dairy farms so its rather unavoidable even if we avoid all dairy. It's also hard to kill and hard to test for it in humans. Even now there is no proper MAP test available but there is researchers trying to make one.
I know there is a MAP vaccine for IBD in the UK in trials right now but its very early days - could be years before we find out much more.
kiny
Well-known member
- Joined
- Apr 28, 2011
- Messages
- 3,480
MAP should be looked it if only because it's a mycobacteria. Tuberculosis is the deadliest bacteria in human history. Any mycobacteria should be regarded as potentially pathogenic in humans and dangerous to human health.
You can actually culture most mycobacteria, with a few caveats. There are mycobacteria that are very dangerous to culture because they are airborne infections risks. A lab needs special permits to culture tuberculosis for example. Some you can't culture in vitro becaus it's so slow growing, like leprea, it takes weeks for leprea to divide. What researches do when they can't grow leprea but want to study it, is the same thing they do with syphilis, they grow it in vivo by infecting an animal.
MAP you can culture. It takes a long time, months, but it's not particularly difficult. The other method is through PCR. I have done both these tests with the help of a veterinary lab which does this testing daily to map the prevalence of paratuberculosis in ruminants. A friend who works in the lab has crohn's disease too. We both did these tests multiple times and were never able to detect MAP, but we could easily detect and grow map from animals with Ptb.
When you get these negative results, or when controlled studies get these negative results where you can't detect MAP at all, the argument is often that intesinal tissue (biopsy) instead of blood should be used to test. But when you do these same blood tests in ruminants, also without access to tissue, there is no problem detecting MAP from ruminants with Ptb.
MAP studies have been plagued by some of these back and forth arguments regarding tissue vs blood testing.
Then there's the question why crohn's disease is not more prevalent among farmers. Just being on farmland or living close to farmland should make one much more likely to develop crohn's disease if MAP is causative, MAP is not just found in feces of animals, it's in the direct environment of farms, it's in aerosol, it's floating above the waterways that lead to farms. But crohn's disease has been quite an urban disease when you go through the studies. The V. Kruiningen clustering of cases in the North of France were urban families, not farm families.
There need to be more studies, if anything because it's a mycobacteria. A mycobacteria in the food chain that kills farm animals should be considered a public health threat, regardless of its zoonotic potential.
You can actually culture most mycobacteria, with a few caveats. There are mycobacteria that are very dangerous to culture because they are airborne infections risks. A lab needs special permits to culture tuberculosis for example. Some you can't culture in vitro becaus it's so slow growing, like leprea, it takes weeks for leprea to divide. What researches do when they can't grow leprea but want to study it, is the same thing they do with syphilis, they grow it in vivo by infecting an animal.
MAP you can culture. It takes a long time, months, but it's not particularly difficult. The other method is through PCR. I have done both these tests with the help of a veterinary lab which does this testing daily to map the prevalence of paratuberculosis in ruminants. A friend who works in the lab has crohn's disease too. We both did these tests multiple times and were never able to detect MAP, but we could easily detect and grow map from animals with Ptb.
When you get these negative results, or when controlled studies get these negative results where you can't detect MAP at all, the argument is often that intesinal tissue (biopsy) instead of blood should be used to test. But when you do these same blood tests in ruminants, also without access to tissue, there is no problem detecting MAP from ruminants with Ptb.
MAP studies have been plagued by some of these back and forth arguments regarding tissue vs blood testing.
Then there's the question why crohn's disease is not more prevalent among farmers. Just being on farmland or living close to farmland should make one much more likely to develop crohn's disease if MAP is causative, MAP is not just found in feces of animals, it's in the direct environment of farms, it's in aerosol, it's floating above the waterways that lead to farms. But crohn's disease has been quite an urban disease when you go through the studies. The V. Kruiningen clustering of cases in the North of France were urban families, not farm families.
There need to be more studies, if anything because it's a mycobacteria. A mycobacteria in the food chain that kills farm animals should be considered a public health threat, regardless of its zoonotic potential.
Last edited:
kiny
Well-known member
- Joined
- Apr 28, 2011
- Messages
- 3,480
Why are certain antibiotics more effective in inducing remission than others. While antibiotics are just used to treat infections complicating crohn's diseae in the West, there is plenty of data on them from the pre-bioligic era and they are still actively used in developing countries to treat crohn's disease. They are also still a good hail mary attempt if medication has failed in people with crohn's disease.
Quinolones are very effective in inducing remission in crohn's disease. They're effective against some non-resistant mycobacteria but they're more effective as a broad spectrum antibiotic that can also kill many foodborne enterobacteriaceae, like E coli and salmonella. Also cell penetrating they can enter active macrophages. If MAP was causative, you wouldn't expect quinolones to be at the top of the chart of effective antibiotics to treat crohn's disease, you would expect another antibiotic there.
Quinolones are very effective in inducing remission in crohn's disease. They're effective against some non-resistant mycobacteria but they're more effective as a broad spectrum antibiotic that can also kill many foodborne enterobacteriaceae, like E coli and salmonella. Also cell penetrating they can enter active macrophages. If MAP was causative, you wouldn't expect quinolones to be at the top of the chart of effective antibiotics to treat crohn's disease, you would expect another antibiotic there.
kiny
Well-known member
- Joined
- Apr 28, 2011
- Messages
- 3,480
And if its due to tolerating, why don't they develop better tasting varieties
Iirc, there's a study where they added vanilla extracts to increase tolerance.
It depends on the EN brand too. 028 tastes bitter due to the protein processing they use, and you need to get used to it to tolerate it daily. Modulen on the other hand is very easy to tolerate, it tastes like sugary milk.
One should be using a straw anyway to drink it, to protect your teeth from the sweetness. I flush my mouth with water afterwards too, or the taste would stay in my mouth all day.
The biggest problem is not the taste I feel. EN don't taste particularly bad, they taste pretty neutral outside of some being bitter, but some enjoy a bitter taste. I think many people fail to adhere to EN because they add in other foods. Not only does that undo EN's effectiveness, it creates a constant craving for those other foods and makes it much harder to adhere to EN.
Telling patients to go on EN, but allowing them to add in solid foods, is like telling an acoholic he needs to stop drinking alcohol, but can have beer on the week-ends. It's not going to work very well.
Last edited:
MAP should be looked it if only because it's a mycobacteria. Tuberculosis is the deadliest bacteria in human history. Any mycobacteria should be regarded as potentially pathogenic in humans and dangerous to human health.
You can actually culture most mycobacteria, with a few caveats. There are mycobacteria that are very dangerous to culture because they are airborne infections risks. A lab needs special permits to culture tuberculosis for example. Some you can't culture in vitro becaus it's so slow growing, like leprea, it takes weeks for leprea to divide. What researches do when they can't grow leprea but want to study it, is the same thing they do with syphilis, they grow it in vivo by infecting an animal.
MAP you can culture. It takes a long time, months, but it's not particularly difficult. The other method is through PCR. I have done both these tests with the help of a veterinary lab which does this testing daily to map the prevalence of paratuberculosis in ruminants. A friend who works in the lab has crohn's disease too. We both did these tests multiple times and were never able to detect MAP, but we could easily detect and grow map from animals with Ptb.
When you get these negative results, or when controlled studies get these negative results where you can't detect MAP at all, the argument is often that intesinal tissue (biopsy) instead of blood should be used to test. But when you do these same blood tests in ruminants, also without access to tissue, there is no problem detecting MAP from ruminants with Ptb.
MAP studies have been plagued by some of these back and forth arguments regarding tissue vs blood testing.
Then there's the question why crohn's disease is not more prevalent among farmers. Just being on farmland or living close to farmland should make one much more likely to develop crohn's disease if MAP is causative, MAP is not just found in feces of animals, it's in the direct environment of farms, it's in aerosol, it's floating above the waterways that lead to farms. But crohn's disease has been quite an urban disease when you go through the studies. The V. Kruiningen clustering of cases in the North of France were urban families, not farm families.
There need to be more studies, if anything because it's a mycobacteria. A mycobacteria in the food chain that kills farm animals should be considered a public health threat, regardless of its zoonotic potential.
Well as you said previous, Crohn's is a catch all term these days and so people with Crohn's might have totally different things going on. So antibiotics works for some because maybe MAP isn't the only possible culprit depending on the type of manifestation you get.
Farmers often pass farms on to their kids, there could be a genetic resilience because those who were sick with IBD in the past, died or sold the farm to some one else who wasn't sick. You still need the genetics to get IBD even if MAP is involved. But also perhaps the exposure of MAP plus all the other bacteria on farms actually creates a balance in their microbiome that urban environments cannot provide.
Surely surgical removal of the inflammed digestive tract can help detect which bacteria the immune system was responding to?
Iirc, there's a study where they added vanilla extracts to increase tolerance.
It depends on the EN brand too. 028 tastes bitter due to the protein processing they use, and you need to get used to it to tolerate it daily. Modulen on the other hand is very easy to tolerate, it tastes like sugary milk.
One should be using a straw anyway to drink it, to protect your teeth from the sweetness. I flush my mouth with water afterwards too, or the taste would stay in my mouth all day.
The biggest problem is not the taste I feel. EN don't taste particularly bad, they taste pretty neutral outside of some being bitter, but some enjoy a bitter taste. I think many people fail to adhere to EN because they add in other foods. Not only does that undo EN's effectiveness, it creates a constant craving for those other foods and makes it much harder to adhere to EN.
Telling patients to go on EN, but allowing them to add in solid foods, is like telling an acoholic he needs to stop drinking alcohol, but can have beer on the week-ends. It's not going to work very well.
True my argument was more that instead of a month of pred you do a month of EN then are given a maintenance drug. If patients lose discipline then i guess prednisone it shall be but they don't seem to even offer EN to most people. I would easily prefer EN over prednisone for a month then transition back to food on a maintenance drug. I will likely ask for it next time and be adamant about it because prednisone sucks.
- Joined
- Apr 24, 2021
- Messages
- 216
Best remission I ever got was from full enn and prednisolene combined.
Ten years on big flair and neither worked had to have a biologic.
There is one key word, crohns is a progressive disease.
That is they keyword my gi told me to rember its "progressive"
Also due to the progression of the disease medications can have less effect on treating and eventually surgery may be required as damaged builds up worse and worse.
But crohns always progresses even past the best biologics we have to date.
Ten years on big flair and neither worked had to have a biologic.
There is one key word, crohns is a progressive disease.
That is they keyword my gi told me to rember its "progressive"
Also due to the progression of the disease medications can have less effect on treating and eventually surgery may be required as damaged builds up worse and worse.
But crohns always progresses even past the best biologics we have to date.
kiny
Well-known member
- Joined
- Apr 28, 2011
- Messages
- 3,480
Surely surgical removal of the inflammed digestive tract can help detect which bacteria the immune system was responding to?
Sort of right.
For MAP there's the challenge that map can simply be transient because it's so widespread in the environment. Just because you detect MAP in tissue by itself doesn't mean much. You need to prove the tissue where MAP was found was consistent with the presence of inflammation, granuloma, and you need to show the immune response was specifically directed at MAP and not any other microbes or antigen in the tissue.
There's this study where MAP was detected in tissue from crohn's disease patients, but also in most controls, later in the study it became clear that the environment where the study was done and samples were taken, contained high number of map. MAP is so widespread in the environment that someone who simply drank tap water, washed their hands and touched tissue, or even aerosol in the air, could have contaminated the tissue.
Btw, this is especially true for fungi, most fungi in the intestine are transient, just someone touching tissue without special gloves will immediately contaminate the sample, because fungi is all over the skin.
These fungi species some studies talk about in reference to crohn's disease are not some exotic fungi. They're Candida spp and Malassezia, they're everywhere, on the skin, in the mouth, in food, etc. They could just be transient in the intestine, they could be sample contamination. They're pathobiont, they're conditionally pathogenic, for most people they generally do not to cause disease.
In the case of AIEC you can't easily do this outside of the people who run the studies who know exactly what they're looking for.
The unsolved challenge in identifying AIEC is to find a simple genetic trait that differentiates it from commensal E Coli to make tests more widespread. While E Coli generally appears in the news when there is a foodborne outbreak, most people harbour E Coli that seems for the most part harmless, either colonized by commensals or transient from food sources. You need to be able to separate invasive E Coli from those commensals.
AIEC is a strain that is not harmless. It has invasive properties. When researchers do these studies where they isolate these strains, they do this based on certain properties AIEC has which allows them to attach to the intestinal wall and invade tissue, they can compare to LF82 reference strains, and they have the time to do this.
Most GI who follow the latest developments will be aware of AIEC, but when a patient asks if they can check a biopsy for the presence of AIEC, they will tell you no. because there is no common genetic marker for identification, and normal lab environments have neither the knowledge or time to do what these studies spend months doing. A lab wants a genetic marker, they want a kit they can buy off the shelves.
Last edited:
kiny
Well-known member
- Joined
- Apr 28, 2011
- Messages
- 3,480
Especially regarding fungi the debate is not easy. The idea that fungi colonize the intestine is not shared by everyone. Fungi live in conditions that you generally don't have in the intestine, the intestine seems too hot, lacking in oxygen and lacking in the type of nutrients fungi rely on in the case of Malassezia.
There's a good argument to be made that the fungi found in the intestine are simply transient. They're from food and the oral cavity and don't "live" in the gut.
Bacteria live in the oral cavity, the ileum and colon. The number of bacteria from the esophagus to the jejunum is tiny compared to the number of bacteria more distally in the ileum and colon.
Not the case when you take biopsies and look for fungi, you can detect them pretty in much more even numbers in the digestive tract, which might indicate they are just passerby from food sources or from ingested saliva from the oral cavity.
This makes that the studies on fungi and crohn's disease are somewhat up in the air. If you can match changes in fungi populatons with a flare, you can then claim these species are responsible for inflammation. But you're not on stable footing when you make that claim, because if fungi are just passerby from food sources, and crohn's disease patients change their eating pattern during flares, the data is completely meaningless.
There's a good argument to be made that the fungi found in the intestine are simply transient. They're from food and the oral cavity and don't "live" in the gut.
Bacteria live in the oral cavity, the ileum and colon. The number of bacteria from the esophagus to the jejunum is tiny compared to the number of bacteria more distally in the ileum and colon.
Not the case when you take biopsies and look for fungi, you can detect them pretty in much more even numbers in the digestive tract, which might indicate they are just passerby from food sources or from ingested saliva from the oral cavity.
This makes that the studies on fungi and crohn's disease are somewhat up in the air. If you can match changes in fungi populatons with a flare, you can then claim these species are responsible for inflammation. But you're not on stable footing when you make that claim, because if fungi are just passerby from food sources, and crohn's disease patients change their eating pattern during flares, the data is completely meaningless.
Last edited:
Especially regarding fungi the debate is not easy. The idea that fungi colonize the intestine is not shared by everyone. Fungi live in conditions that you generally don't have in the intestine, the intestine seems too hot, lacking in oxygen and lacking in the type of nutrients fungi rely on in the case of Malassezia.
There's a good argument to be made that the fungi found in the intestine are simply transient. They're from food and the oral cavity and don't "live" in the gut.
Bacteria live in the oral cavity, the ileum and colon. The number of bacteria from the esophagus to the jejunum is tiny compared to the number of bacteria more distally in the ileum and colon.
Not the case when you take biopsies and look for fungi, you can detect them pretty in much more even numbers in the digestive tract, which might indicate they are just passerby from food sources or from ingested saliva from the oral cavity.
This makes that the studies on fungi and crohn's disease are somewhat up in the air. If you can match changes in fungi populatons with a flare, you can then claim these species are responsible for inflammation. But you're not on stable footing when you make that claim, because if fungi are just passerby from food sources, and crohn's disease patients change their eating pattern during flares, the data is completely meaningless.
Regarding this part: If you can match changes in fungi populatons with a flare
Could you not do the opposite and give medication to treat the fungi or bacteria to see if there is a faster improvement in the flares than a control group who do not take it. We can see prednisone improves flares rapidly and EEN without needing to sample. We might not be able to identify specifically which bacteria or fungi but the improvement would show where to look.
arent there beneficial bacteria that oppose fungi/candida? it's my understanding that fungi and bacteria compete with each other and have methods to reduce each other's sway in the soup. following that logic, wouldn't it work to treat fungi overgrowth with bacteria, and bacterial overgrowth with fungi? 'rebalancing' the whole...
Similar threads
- Replies
- 4
- Views
- 2K
- Replies
- 0
- Views
- 561
- Replies
- 2
- Views
- 1K
- Replies
- 0
- Views
- 881